When John came to me for treatment, he’d lost his job a year earlier; at 58 years old he was not optimistic about finding a new one. Since then, he’d stopped exercising, his diet had deteriorated and he’d had a recent health scare. His relationships were also suffering, as he often argued with his wife, felt alienated from his adult children and rarely got together with his friends. He felt broken, and sometimes wondered if life was worth living.
Like what you are reading? For more stimulating stories, thought-provoking articles and new video announcements, sign up for our monthly newsletter.
John’s situation is not at all uncommon. As one part of our life suffers, others often go down with it. What might start as a physical illness soon affects our minds, just as a psychological stressor like losing one’s job can lead to physical exhaustion and poor health. The cascade can continue and affect us at our core, leaving us feeling lost and dispirited.
I’m well acquainted with this downward spiral not only from my clinical work but from my own extended physical illness that resulted in social isolation and a major depressive episode. Eventually I felt like a burden to everyone and wondered if my family would be better off without me.
Just as our struggles often spread into many areas of our lives, our healing requires a multi-faceted response. My own approach as a therapist integrates cognitive behavioral therapy (CBT) with mindfulness, which I call “Think Act Be.” It’s a simple reminder of three interconnected paths to healing—Mind, Body, and Spirit (see figure).
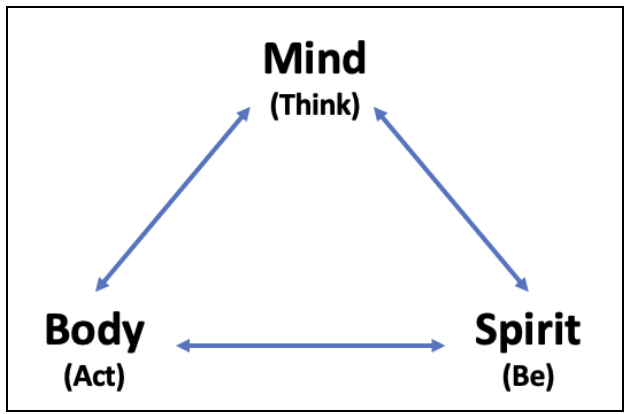 When I’m working with clients I often ask myself which of these paths might be most helpful to them at this point in their treatment.
When I’m working with clients I often ask myself which of these paths might be most helpful to them at this point in their treatment.- Are their thoughts serving them well?
- Are their actions consistently rewarding them with enjoyment and a feeling of accomplishment?
- Do they find meaning and connection to nourish their spirits?
Other clinicians before me have recognized the power of combining these three schools of thought (e.g., Mindfulness-Based Cognitive Therapy). Indeed, integrative approaches in general are commonly used by clinicians, whether or not they follow a CBT approach. Therapists of all stripes see the value in treating the whole person.
Bringing the Principles to Life
The principles of mindfulness-based CBT are very straightforward and easy to explain:
Foster healthy thinking.
Do life-giving activities.
Practice present awareness.
The challenge lies in bringing these principles to life, otherwise they’re no more effective than easy truisms like “be in the moment.” How do we retrain our minds? Which activities are the right ones for me? What are ways to practice mindful awareness?
In my experience, three ingredients are necessary to develop new and more effective habits that promote healing:
- A clear and focused plan
- Daily practice
- A wide range of practices
In general, it’s best if the plan is written, which makes it much easier to remember and provides greater accountability. Some therapists write the plan on an index card so it’s easy for the client to carry it with them. That idea inspired me to develop The CBT Deck, a deck of cards printed with daily CBT and mindfulness-based practices. It includes many of the same techniques that John and I worked on during his treatment; example exercises from the deck are included in bold in the following discussion of his treatment and recovery.
John’s Recovery
In my work with John, we focused first on adding valued activities back into his life because this seemed like an area of “low hanging fruit,” and behavioral activation tends to pay off quickly. His activities included going on weekend adventures with his wife and doing fun things that also provided physical movement.
 We also worked toward taking care of tasks around the house that he’d been putting off and on building positive interactions with others since his relationships had suffered. Given his health challenges, we worked on ways to improve his sleep and eat more healthfully.
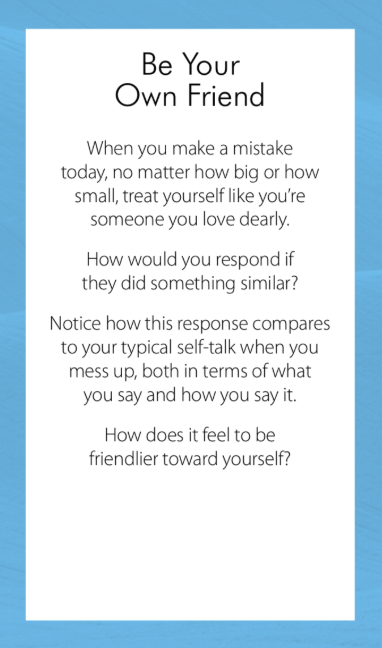
We also worked toward taking care of tasks around the house that he’d been putting off and on building positive interactions with others since his relationships had suffered. Given his health challenges, we worked on ways to improve his sleep and eat more healthfully.Soon we began addressing his thoughts, starting with recognizing thoughts as thoughts. He identified an overly negative self-critical voice that told him he was “unwanted” and “useless,” which we worked to correct in various situations (see sample card).
Mindfulness became the third pillar of John’s treatment and recovery. Through different meditation practices he learned to quiet his mind and recognize its chatter, and could prevent himself from getting caught up in negative trains of thought. He also found relief from putting up less resistance to reality, instead opening to the unpredictability of life.
We worked together to bring these practices into his daily life and his interactions with others. Gratitude was also an important part of John’s recovery, as he started to notice how much was right in his life.
It was only a few weeks before John was feeling markedly better. That said, the improvements were somewhat delayed; he didn’t feel immediately better after the first weekend outing with his wife, and his mindset didn’t change miraculously after one week of working on his thoughts. Just as giving up life activities took a while to affect John’s well-being, so the effects of resuming them were somewhat delayed. This delay is part of why consistent practice is important; if a person stops the practice after a day or two, they probably won’t have gotten a sufficient “dose” to see real improvement—and may conclude prematurely that “it didn’t work for me.”
John and I met weekly for more than a year as the improvements continued. Eventually we tapered down to meeting about once a month, which John finds helpful to maintain the practices that keep him well.
Healing for All
After many rounds of inconclusive medical tests, I began to accept that a mind-body-spirit approach to healing was just as relevant for me as for those I was treating:
Think: I’ve found it extremely helpful to make simple adjustments to my mindset—for example, seeing myself as “still healing” rather than “still sick.”
Act: I threw myself into life-giving activities like gardening, where I can see the fruits (and vegetables) of my labor.
Be: I’ve given myself space to connect with deeper parts of myself that I’d forgotten about, including a renewed connection to sacred scriptures.
It might sound funny, but I plan to use The CBT Deck myself as a regular reminder of the kinds of practices that enrich our lives.
As you assist others in healing—or work toward your own—what framework do you find most helpful? In what way does your approach tend to the mind, body, and spirit?
File under: The Art of Psychotherapy



